Over 75% of children with cerebral palsy (CP) have spasticity. While treatments such as selective dorsal rhizotomy, baclofen, and botulinum toxin injections are common and can reduce spasticity, recent evidence suggests these procedures may have undesirable side effects and long-term detrimental effects on neuromuscular development.
New options are needed to reduce spasticity, support neuroplasticity, and improve function for children with CP and understand its impact on mobility and function.
Our multidisciplinary team completed a cross-over pilot study to evaluate the impacts of noninvasive spinal stimulation on spasticity for children with CP. Since tSCS is theorized to amplify afferent signals during functional activities, we paired spinal stimulation with short-burst locomotor treadmill training (SBLTT), a gait training protocol designed specifically for children with CP that mimics child walking patterns. SBLTT has been shown to improve walking function for children with CP, providing individualized and intense variable mass walking practice.
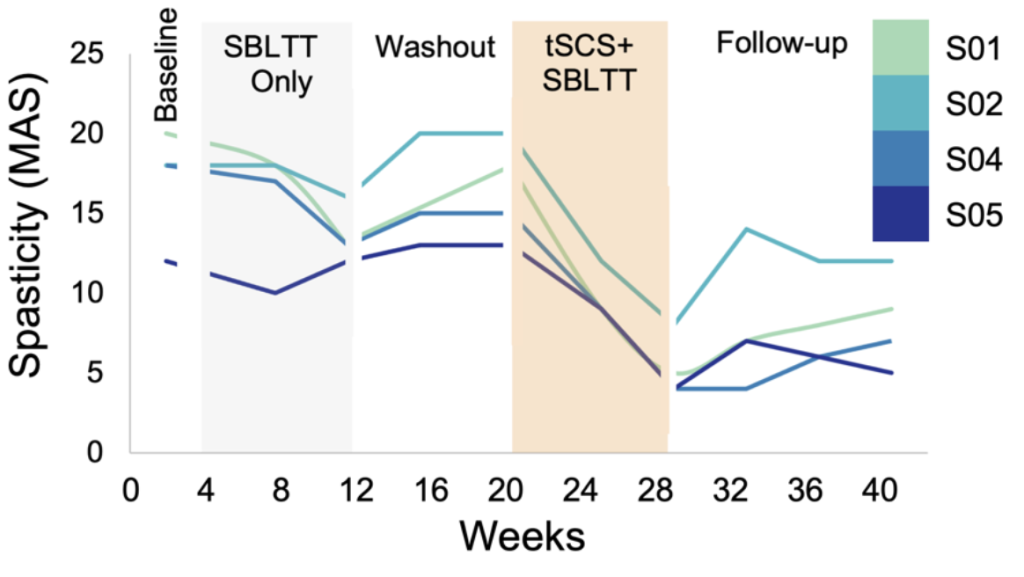
Excitingly, in our pilot we found that all four children with CP (ages 4-13 years) had 2- to 3-fold less spasticity after 24 sessions of SBLTT with tSCS compared to 24 sessions of SBLTT alone. Further, spasticity was nearly eliminated in key muscle groups, including the hamstrings and ankle plantarflexors, and was sustained for at least three months. Other groups have also reported that a single session of tSCS may reduce co-contraction and that sixteen sessions of tSCS with activity-based neurorehabilitation may improve gross motor function in CP.
Learn more about these results led by PhD-alumna Charlotte DeVol from Mechanical Engineering and Siddhi Shrivastav from Rehabilitation Medicine in our publication in IEEE Transactions on Biomedical Engineering and a deep dive into the biomechanical changes in Gait & Posture.
Our Team
This project brings together a team with expertise in physical therapy, neuroscience, and engineering. Collaborators include Kristie Bjornson from Seattle Children’s Research Institute, Chet Moritz from UW Electrical & Computer Engineering, & Heather Feldner from UW Rehabilitation Medicine.
Acknowledgements
We thank the children and their families for the time they dedicated to this research. We also thank Soshi Samejima, Fatma Inanici, Rich Henderson, and Lauren Bachman for assisting with interventions and assessments, and Avocet Nagle Christensen for data analysis.
Funding
This work was supported by Seattle Children’s Hospital CP Research Pilot Study Fund 2020 Award, UW Rehabilitation Medicine Walter C. and Anita C. Stolov 2021 Research Fund, and NSF Graduate Research Fellowship Program Award DGE-1762114. Chet Moritz serves as a clinical advisor to the company SpineX, who provided the stimulator for the study.