A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy, University of Washington, 2016. To download and read in full, CLICK HERE. to access through the University of Washington’s ResearchWorks Archive.
 Background: Many individuals with cerebral palsy (CP) and stroke are prescribed ankle foot orthoses
Background: Many individuals with cerebral palsy (CP) and stroke are prescribed ankle foot orthoses
(AFOs) for use during daily life. AFOs have been shown to improve pathologic gait and walking
speed in CP and stroke by providing support and alignment. There are many different types of
AFOs available such as posterior leaf spring AFOs, rigid AFOs, and articulated AFOs. Further,
there are many parameters that can be customized or tuned for each type of AFO, such as
stiffness, heel height, shank to vertical angle, and foot plate length. However, how different types
of AFOs and the customization of specific parameters impact muscle function remains unclear.
Purpose: The goals of this dissertation were to evaluate how different types of AFOs and different
tuning parameters impact gait kinematics and muscle function. Of particular interest is the
gastrocnemius, a key muscle that crosses the knee and ankle joints and is commonly tight among
individuals with CP or stroke. Gastrocnemius operating length, defined as the total muscle and
tendon length during a functional activity, influences ankle and knee kinematics during gait.
Results/Discussion: This dissertation provides important evidence for how humans adapt to various AFO
properties and suggests important implications for the design and prescription of AFOs. This
work provides a quantitative evaluation of how AFOs impact musculotendon dynamics among
individuals with stroke (Aim 1) and cerebral palsy (Aim 2). The fabrication methods in Aim 3
creates a powerful and flexible research platform for evaluating AFO design, which may be
extended to fabrication of AFOs for daily use with further improvements in additive
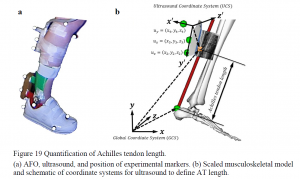
manufacturing materials and methods. The final study (Aim 4), provides the first experimental
evidence combining ultrasound and musculoskeletal modeling to understand how muscle and
tendon length are impacted by AFO design. These evaluations provide guidance for future AFO
design and prescription that can not only augment human mobility for unimpaired individuals,
but also provide improve metrics for improving function and guiding rehabilitation for
individuals with neurologic impairments.
