Journal Article in Sensors
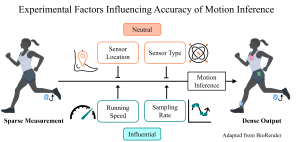
Inertial measurement units (IMUs) are used to analyze running performance. While leveraging one sensor to estimate kinematic and kinetic variables is common, sparsity limits the number of digital biomarkers that can be evaluated.
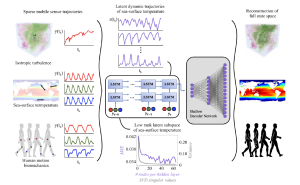
 Aim: Shallow recurrent decoder networks (SHRED) can reconstruct a dense set of time-series signals from a single input sensor and have been successful in human mobility applications, highlighting the potential for this algorithm to monitor running.
Aim: Shallow recurrent decoder networks (SHRED) can reconstruct a dense set of time-series signals from a single input sensor and have been successful in human mobility applications, highlighting the potential for this algorithm to monitor running.
Methods: We trained and tested subject-specific SHRED models of nine subjects running on a treadmill to map from one input sensor to the remaining three IMUs. We varied the type of input to reflect experimental parameters that are important in running studies—sensor location, sensor type, sampling rate, and running speed—and compared the error of inferred signals from each input type.
Results: Sensor location and type did not impact SHRED inference accuracy, while decreasing the sampling rate affected the accuracy of ankle measurements. All ankle acceleration inferences from these models remained below the minimal detectable change threshold of 12.0 m/s2. SHRED models trained and tested at multiple speeds did not accurately infer IMU measurements below this threshold.
Interpretation: SHRED may broaden the scope of motion analysis by expanding access to data with fewer sensors. The data from this study and an instructional Jupyter notebook for training and testing individualized SHRED models are available at [link to GitHub].