Journal article in Journal of Biomechanics:
In collaboration with Gillette Children’s Specialty Healthcare, we evaluated whether muscle synergies change when unimpaired individuals walk at different speeds and slopes.
 Background: The aim of this study was to determine whether changes in synergies relate to changes in gait while walking on a treadmill at multiple speeds and slopes. The hypothesis was that significant changes in movement pattern would not be accompanied by significant changes in synergies, suggesting that synergies are not dependent on the mechanical constraints but are instead neurological in origin.
Background: The aim of this study was to determine whether changes in synergies relate to changes in gait while walking on a treadmill at multiple speeds and slopes. The hypothesis was that significant changes in movement pattern would not be accompanied by significant changes in synergies, suggesting that synergies are not dependent on the mechanical constraints but are instead neurological in origin.
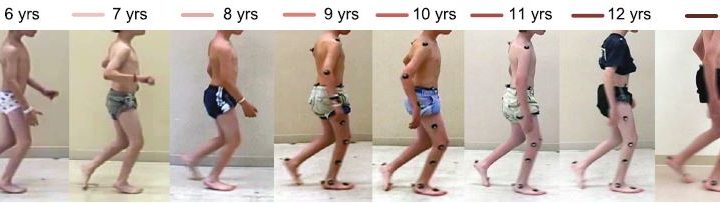
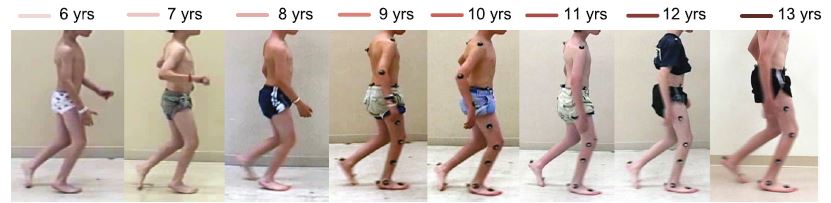
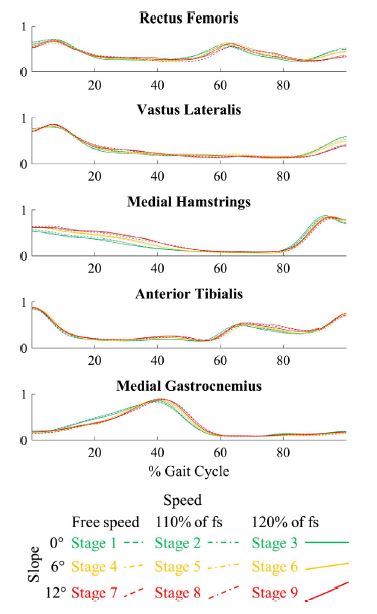
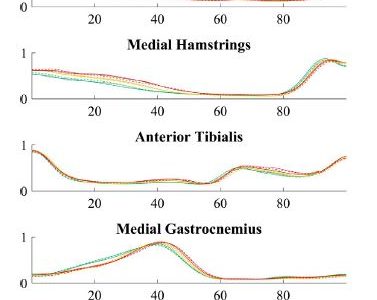
Methods: Sixteen typically developing children walked on a treadmill for nine combinations (stages) of different speeds and slopes while simultaneously collecting kinematics, kinetics, and surface electromyography (EMG) data. The kinematics for each stride were summarized using a modified version of the Gait Deviation Index that only includes the sagittal plane. The kinetics for each stride were summarized using a modified version of the Gait Deviation Index – Kinetic which includes sagittal plane moments and powers. Within each synergy group, the correlations of the synergies were calculated between the treadmill stages.
Results: While kinematics and kinetics were significantly altered at the highest slope compared to level ground when walking on a treadmill, synergies were similar across stages.
Conclusions: The high correlations between synergies across stages indicate that neuromuscular control strategies do not change as children walk at different speeds and slopes on a treadmill. However, the multiple significant differences in kinematics and kinetics between stages indicate real differences in movement pattern. This supports the theory that synergies are neurological in origin and not simply a response to the biomechanical task constraints.

 This award will support clinical trials with 10 kids with CP trying PlayGaitTM in Spring and Summer 2017 along with two quarters of Research Assistant support.
This award will support clinical trials with 10 kids with CP trying PlayGaitTM in Spring and Summer 2017 along with two quarters of Research Assistant support.