Congratulations to Nicole Zaino and our colleague Mike Schwartz at Gillette Children’s Specialty Healthcare for both being nominated as finalists for the Best Presentation Award at the upcoming ESMAC Conference in Amsterdam. Their abstracts are among the top 16 submissions to the conference and the final award will be determined based upon their presentations.

Nicole will be presenting her research:
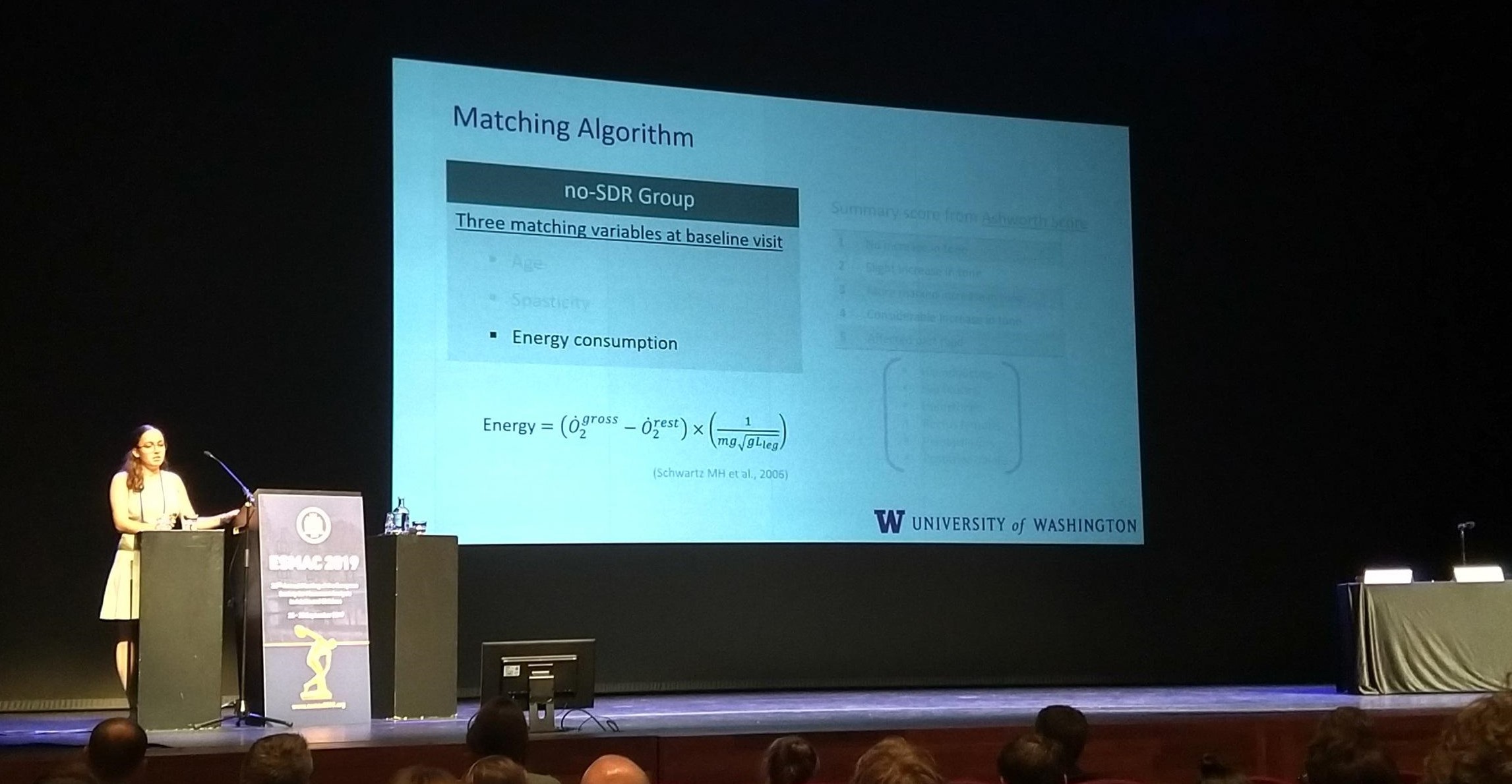
Spasticity reduction in children with cerebral palsy is not associated with reduced energy during walking
Selective dorsal rhizotomy reduces spasticity, but does it also reduce energy consumption during walking? In an analysis of over 300 children with cerebral palsy, Nicole demonstrated that although rhiztomy does reduce spasticity, it does not reduce energy consumption. These results provide further evidence that spasticity is not a main contributor to elevated energy among people with cerebral palsy. You can also learn more about this study from our recent submitted manuscript, available on bioRxiv.
Mike will be presenting his research:
The effects of walking speed and age on energy consumption in children with cerebral palsy and their typically developing peers
We know that walking energy is high among people with cerebral palsy, and that energy varies with speed and age. Using retrospective data of over 300 kids with cerebral palsy and 150 typically-developing peers, Mike used a statistical model to evaluate these speed and age effects. He found that energy decreases until 8-10 years of age for kids with CP, while it remains stable beyond age 5 for typically-developing peers. Kids with CP also have a greater elevation in energy with greater walking speeds. These results are important to help quantify and understand impacts of interventions, like surgery or assistive devices, which are often done during this time period when kids are still growing and developing.
They will both be presenting in the Optimizing Energy Cost session from 11:40-12:30 on Thursday, September 26th.
Best of luck to Nicole & Mike!