Journal Article in Assistive Technology:
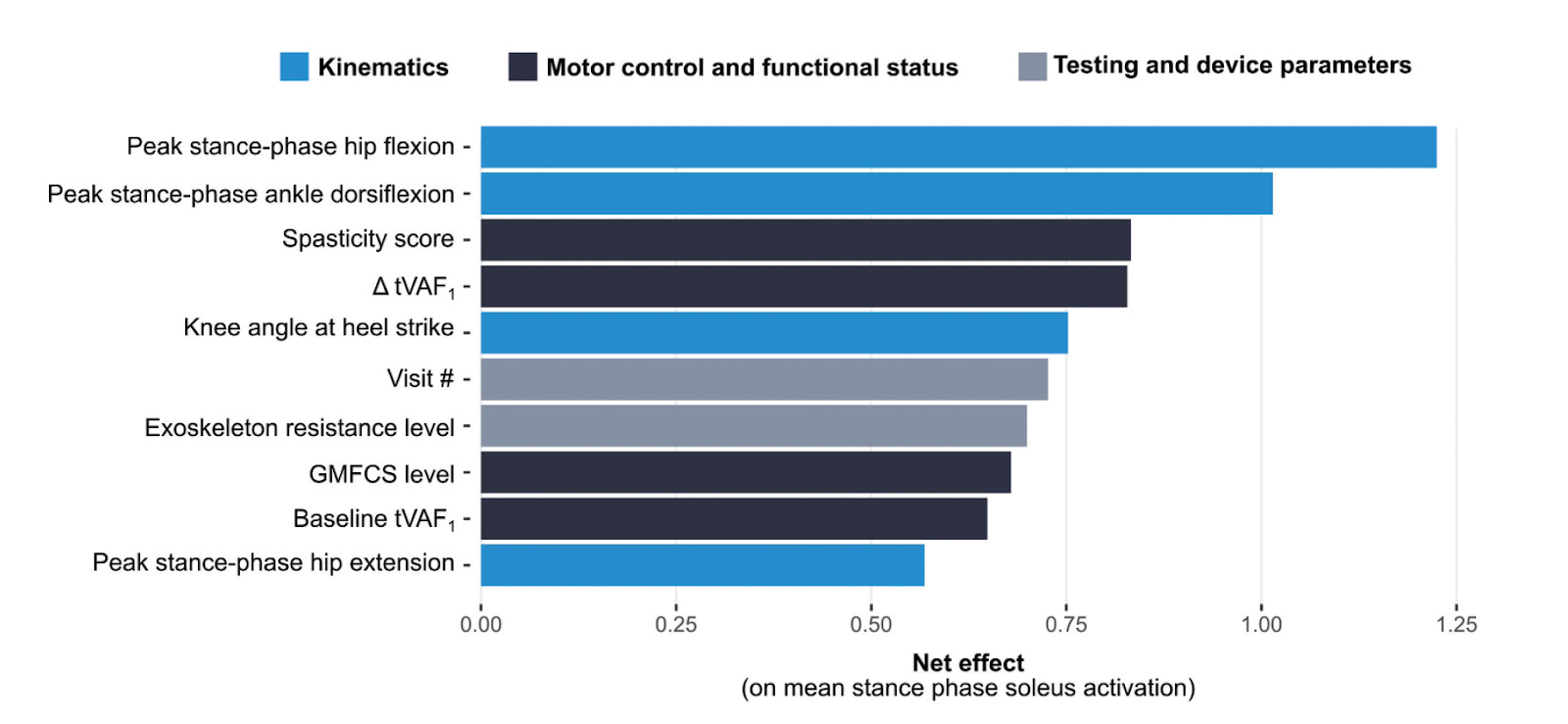
Our findings underscored the importance of monitoring how users change their gait kinematics when walking with the resistive device, with a specific emphasis on stance-phase lower limb extension. We also highlight the necessity of considering an individual’s functional status and amount of practice with the device, as well as more obvious factors, like device parameters. BART can be used early in the development of robotic gait training interventions to better understand complex and multifactorial user-device interactions.
Aim: Although ankle exoskeletons offer a promising means of augmenting gait training and enhancing independent mobility among individuals with neuromuscular disorders, response to existing paradigms is highly heterogeneous. In this study we aimed to identify factors which may affect how individuals with cerebral palsy (CP) interact with a resistive ankle exoskeleton during multi-day training to inform future device design and individualized tuning.
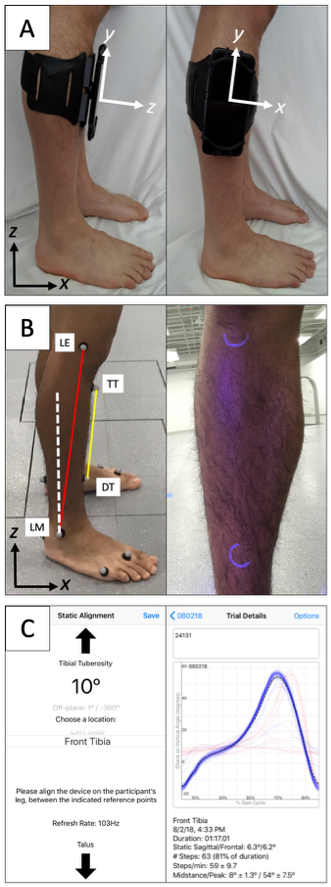
Method:We evaluated the gait mechanics (kinematics and muscle activity) of eight individuals with CP as they walked with bilateral ankle exoskeletons – designed to promote increased plantar flexor recruitment – during a seven-day training paradigm. These data along with pertinent device and participant parameters were input into a Bayesian Additive Regression Trees (BART) machine learning model to identify factors which were most associated with increased plantar flexor recruitment.
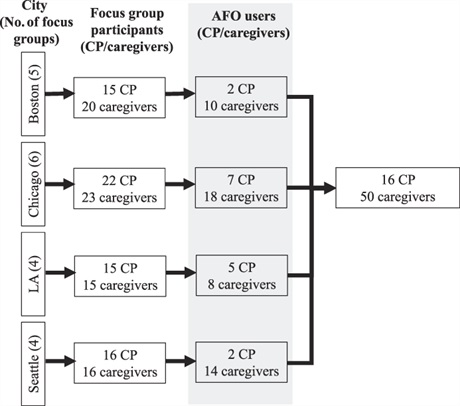
Results: Four themes emerged: 1) AFO provision is a confusing and lengthy process, 2) participants want more information during AFO provision, 3) AFOs are uncomfortable and difficult to use, and 4) AFOs can benefit mobility and independence. Caregivers and individuals with CP recommended ideas such as 3D printing orthoses and education for caregivers on design choices to improve AFO design and provision.
Interpretation: Individuals with CP and their caregivers found the AFO provision process frustrating but highlight that AFOs support mobility and participation. Further opportunities exist to support function and participation of people with CP by streamlining AFO provision processes, creating educational materials, and improving AFO design for comfort and ease of use.