The University of Washington College of Engineering re-launched Engineering Discovery Days this spring. Discovery Days has been a signature outreach event for over 100 years, providing fun and enriching hands-on experiences for students, teachers, and families from across the state. Discovery Days is also an opportunity for our community of UW Engineering students, staff, and faculty to share their passion for engineering with the next generation of innovators.
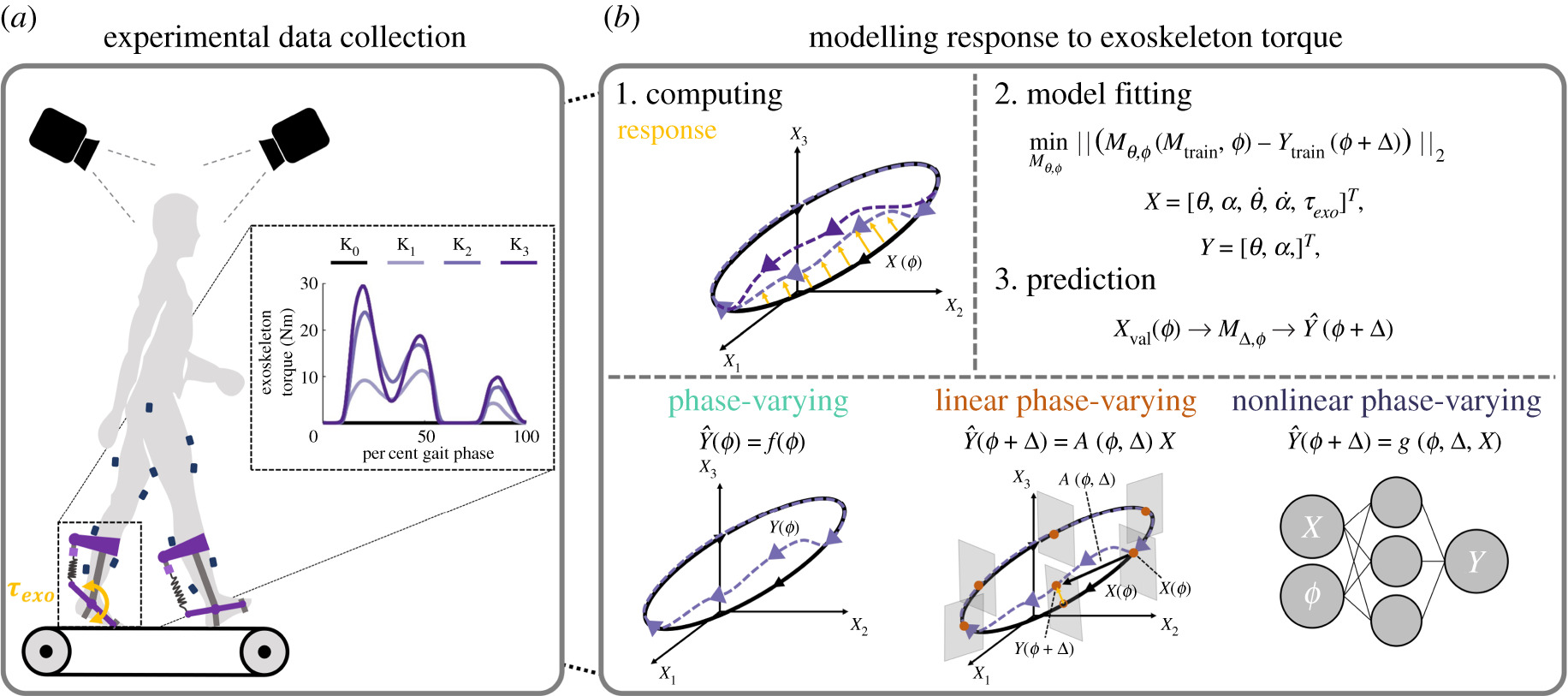
The UW Biomechanics Faculty put together an exhibit titled “Biomechanics Assemble! From Exoskeletons to Cytoskeletons” with the goal of demonstrating how we study movement and forces in humans and cells at UW.








The Steele Lab along with the Ingraham Lab hosted two booths. Each booth featured hand-on activities and games for students to engage with.
The first booth features an ensemble of exoskeletons and assistive devices, including the Biomotum Spark and 3D printed prosthetic hands.
The second booth featured two games for students to engage with, including “Myodino” using Delsys EMG sensors, and “UltraLeap Ring Sorting” VR game using the UltraLeap hand tracking technology.
In this lab, we think the human body is “The Ultimate Machine” and we were so excited to share HOW we study the human body at Discovery Days 2024.