Journal article in PLOS ONE:
Michael Rosenberg and Kat Steele investigate the impacts of ankle foot orthoses on children with cerebral palsy and typically-developing peers through simulation.
Background
Passive ankle foot orthoses (AFOs) are often prescribed for children with cerebral palsy (CP) to assist locomotion, but predicting how specific device designs will impact energetic demand during gait remains challenging. Powered AFOs have been shown to reduce energy costs of walking in unimpaired adults more than passive AFOs, but have not been tested in children with CP.
Aim
The goal of this study was to investigate the potential impact of powered and passive AFOs on muscle demand and recruitment in children with CP and crouch gait.
Method
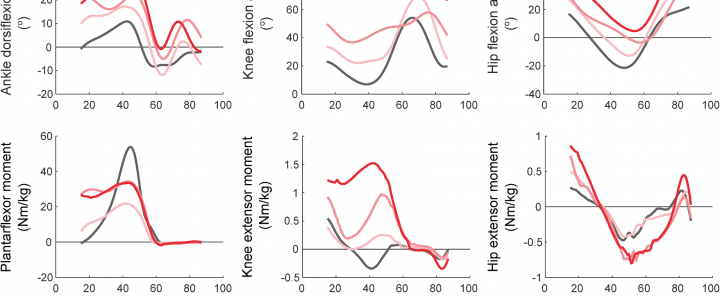
We simulated gait for nine children with crouch gait and three typically-developing children with powered and passive AFOs. For each AFO design, we computed reductions in muscle demand compared to unassisted gait.
Results
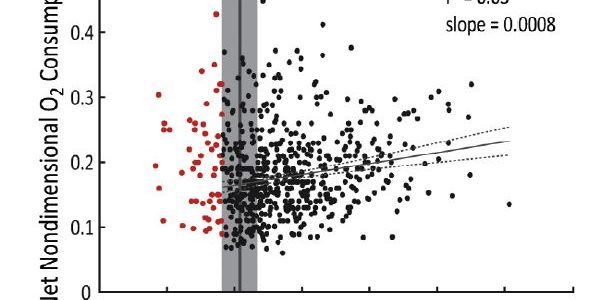
Powered AFOs reduced muscle demand 15–44% compared to unassisted walking, 1–14% more than passive AFOs. A slower walking speed was associated with smaller reductions in absolute muscle demand for all AFOs (r2 = 0.60–0.70). However, reductions in muscle demand were only moderately correlated with crouch severity (r2 = 0.40–0.43). The ankle plantarflexor muscles were most heavily impacted by the AFOs, with gastrocnemius recruitment decreasing 13–73% and correlating with increasing knee flexor moments (r2 = 0.29–0.91).
Interpretation
These findings support the potential use of powered AFOs for children with crouch gait, and highlight how subject-specific kinematics and kinetics may influence muscle demand and recruitment to inform AFO design. PDF