Journal Article in Journal of NeuroEngineering and Rehabilitation
Biofeedback is a promising noninvasive strategy to enhance gait training among individuals with cerebral palsy (CP). Commonly, biofeedback systems are designed to guide movement correction using audio, visual, or sensorimotor (i.e., tactile or proprioceptive) cues, each of which has demonstrated measurable success in CP.
Aim: The aim of this study is to evaluate how the modality of biofeedback may influence user response which has significant implications if systems are to be consistently adopted into clinical care.
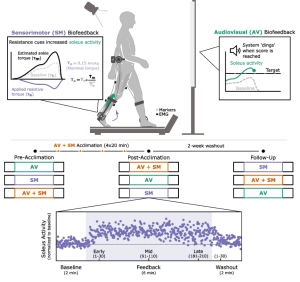
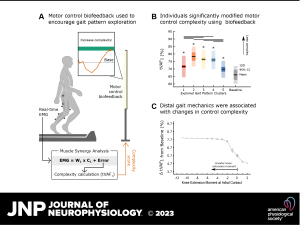
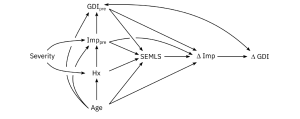
Method: In this study, we evaluated the extent to which adolescents with CP (7M/1F; 14 [12.5,15.5] years) adapted their gait patterns during treadmill walking (6 min/modality) with audiovisual (AV), sensorimotor (SM), and combined AV + SM biofeedback before and after four acclimation sessions (20 min/session) and at a two-week follow-up. Both biofeedback systems were designed to target plantarflexor activity on the more-affected limb, as these muscles are commonly impaired in CP and impact walking function. SM biofeedback was administered using a resistive ankle exoskeleton and AV biofeedback displayed soleus activity from electromyography recordings during gait. At every visit, we measured the time-course response to each biofeedback modality to understand how the rate and magnitude of gait adaptation differed between modalities and following acclimation.
Results: Participants significantly increased soleus activity from baseline using AV + SM (42.8% [15.1, 59.6]), AV (28.5% [19.2, 58.5]), and SM (10.3% [3.2, 15.2]) biofeedback, but the rate of soleus adaptation was faster using AV + SM biofeedback than either modality alone. Further, SM-only biofeedback produced small initial increases in plantarflexor activity, but these responses were transient within and across sessions (p > 0.11). Following multi-session acclimation and at the two-week follow-up, responses to AV and AV + SM biofeedback were maintained.
Interpretation: This study demonstrated that AV biofeedback was critical to increase plantarflexor engagement during walking, but that combining AV and SM modalities further amplified the rate of gait adaptation. Beyond improving our understanding of how individuals may differentially prioritize distinct forms of afferent information, outcomes from this study may inform the design and selection of biofeedback systems for use in clinical care.