Congratulations to Spencer Hensley, who has been selected for a Mary Gates Research Scholarship! This highly competitive University of Washington program supports undergraduate students as they deepen their engagement in research while working closely with faculty mentors.
The Mary Gates Research Scholarship is designed to enhance students’ educational experiences by giving them the resources to devote more time and focus to their research. With reduced financial pressure, scholars are able to pursue more ambitious questions, develop new skills, and contribute meaningfully to their fields.
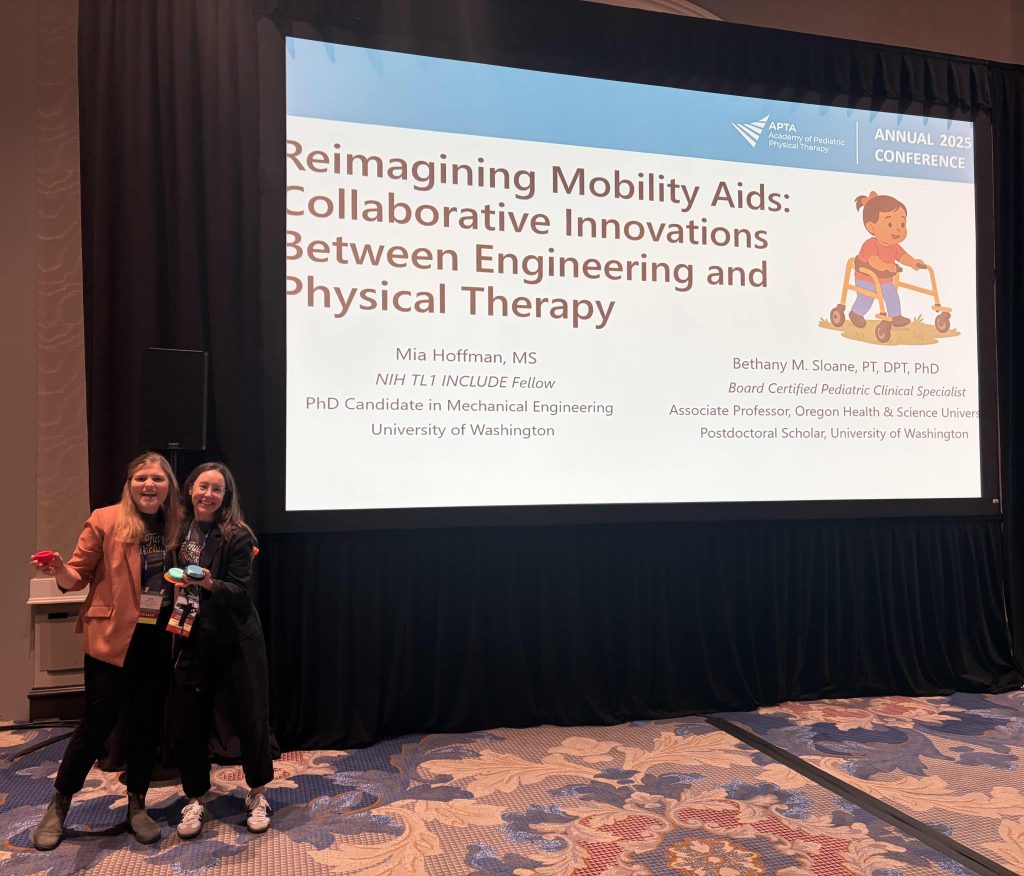
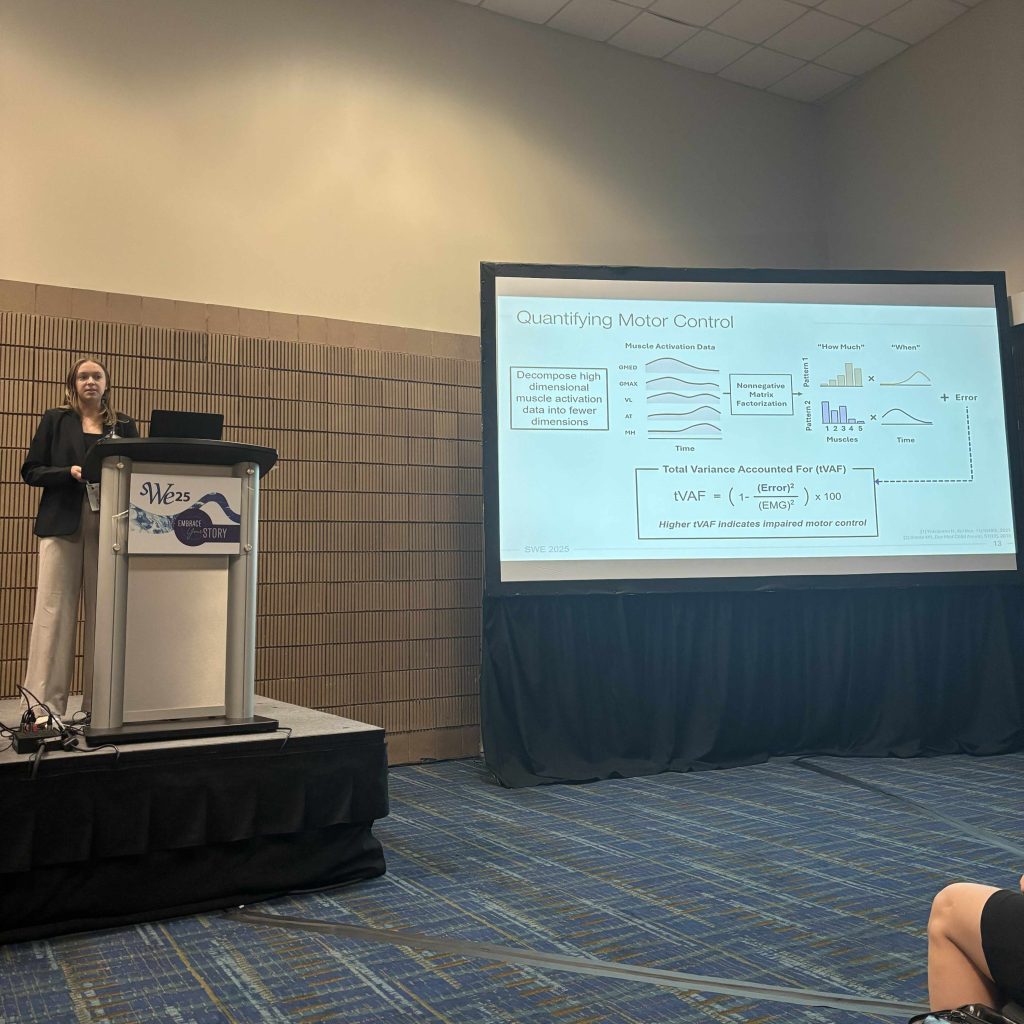
In the Neuromechanics and Mobility Lab, Spencer supports Mia Hoffman’s research on mobility aids for children with Down syndrome and other gross motor delays, contributing to efforts to understand how early access to mobility devices supports participation and development.
Please join us in celebrating this achievement – way to go, Spencer!