Journal Article in IEEE Transactions on Biomedical Engineering
Non-invasive neuromodulation may be an alternative approach that can improve outcomes in CP when combined with physical therapy. Transcutaneous spinal cord stimulation (tSCS) is a novel, non-invasive neuromodulation technique that can modulate spinal and supraspinal circuits especially when implemented with physical therapy.
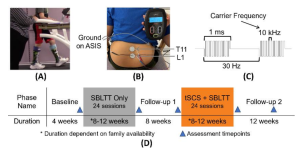
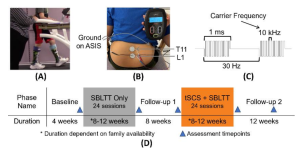 Aim: The purpose of this pilot study was to evaluate the effects of transcutaneous spinal cord stimulation (tSCS) and short-burst interval locomotor treadmill training (SBLTT) on spasticity and mobility in children with cerebral palsy (CP).
Aim: The purpose of this pilot study was to evaluate the effects of transcutaneous spinal cord stimulation (tSCS) and short-burst interval locomotor treadmill training (SBLTT) on spasticity and mobility in children with cerebral palsy (CP).
Methods: We employed a single-arm design with two interventions: SBLTT only, and tSCS + SBLTT, in four children with CP. Children received 24-sessions each of SBLTT only and tSCS + SBLTT. Spasticity, neuromuscular coordination, and walking function were evaluated before, immediately after, and 8- weeks following each intervention.
Results: Spasticity, measured via the Modified Ashworth Scale (MAS), reduced in four lower extremity muscles after tSCS + SBLTT (1.40 ± 0.22,) more than following SBLTT only (0.43 ± 0.39). One-minute walk test (1-MWT) distance was maintained during both interventions. tSCS + SBLTT led to improvements in peak hip and knee peak extension (4.9 ± 7.3° and 6.5 ± 7.7°), that drove increases in joint dynamic range of 4.3 ± 2.4° and 3.8 ± 8.7° at the hip and knee, respectively. Children and parents reported reduction in fatigue and improved gait outcomes after tSCS + SBLTT. Improvements in spasticity and walking function were sustained for 8-weeks after tSCS + SBLTT.
Interpretation: These preliminary results suggest that tSCS + SBLTT may improve spasticity while simultaneously maintaining neuromuscular coordination and walking function in ambulatory children with CP. This work provides preliminary evidence on the effects of tSCS and the combination of tSCS + SBLTT in children with CP.